Imagine an STI that you can’t treat. You go from doctor to doctor, from pill to pill, but nothing can clean out your undercarriage. The infection starts to spread. Like the one-night-stand you contracted it from, the infection refuses to leave after you make it clear that “we’re done here”.
Bacteria can get into your body in many ways. In fact, you’re crawling with bacteria as you read this, most of which are either completely harmless or genuinely beneficial. You can’t live without them. But there are harmful bacteria, too, and for these we have a secret weapon. Antibiotics revolutionised the world when they became available in the 1930’s: they’ve made the world a place in which you can safely heal from trauma, and you don’t need to have six kids in the hopes that at least three may grow old enough to till the cornfields. But it’s been a double-edged sword.
Every time you take antibiotics, the drugs work their way through your system, stifling populations of bacteria inside you – the good, and the bad. This is great for infections, it means that your body has a much higher chance of surviving. But it comes at a cost. There is a small chance that even just one bacterium inside you will possess some mutation, some genetic trick, that renders it immune to the antibiotics you’ve just taken. It survives the medicinal onslaught, and its children inherit its genetic immunity to the antibiotics. This is bad news. This is how we end up with strains of bacterial infections that cannot be treated by antibiotics. And, yes, this potentially includes several STI’s. It can also include infamous infections like Bubonic Plague, or Tuberculosis, which used to have the charming moniker of “The Consumption”. Doesn’t sound like something you want to come down with, does it?
There has only been one case of antibiotic-resistant Tuberculosis in New Zealand. Can you guess where? It was here, in Dunedin. The man infected with this strain was treated at the cost of $10,000 a month. Drugs had to be flown in from the U.S. to treat him when our stocks ran out, and this is just for one person. He made a full recovery, but as the rate of antibiotic prescriptions continues to go up, so too do the rates of resistant strains.
Brian, a recent graduate from Otago, works with people who studied this field at Uni. He told Critic that antibiotic resistance was a bigger problem than it’s been since 1930, when the drugs were invented. And speaking of inventions, new antibiotics can’t just be churned out of a lab at the drop of a hat. “There is not a single class of antibiotics that we have created ourselves”, said Brian. “Every last one of them was first identified in a fungus and then appropriated for human use.” As humans continue to push out to the untouched regions of the planet, we extend what Brian called “a fingerprint that degrades diverse ecosystems and that costs us opportunities to take these molecules and these drugs and use them [for our benefit].” We cannot simply create antibiotics, we have to learn them from nature. And as we continue to chop away at that nature, we will continue to lose potential medicines before they’re ever given a chance to be helpful.
In the meantime, while we continue to prescribe antibiotics, human error is building a veritable army of treatment-resistant bacteria. Every time you don’t finish your prescribed course, the few most resilient stragglers are allowed to multiply, and their progeny is that much stronger in the face of future treatment. These bacteria can cause illnesses like TB, sure, but they can also be responsible for many of the sexually-transmitted diseases that we can dismiss as an “oopsie” today.
Take Syphilis, for example. Syphilis, in its later stages, can enter your brain. Al Capone had it, and towards the end of his life, he was basically insane. It actually became uncool to be associated with the most notorious American gangster of the day, even amongst his fellow inmates on Alcatraz. He completely lost the plot because of untreated Syphilis. Syphilis can also “fuck with your bones”, according to Brian, and would be an absolute nightmare if suddenly resistent to treatment. “Part of this new era that we’re going into is that you will have untreatable STI’s again”, said Brian, “and that’s terrible. As a society, I think we’ve forgotten what it’s like to have those.”
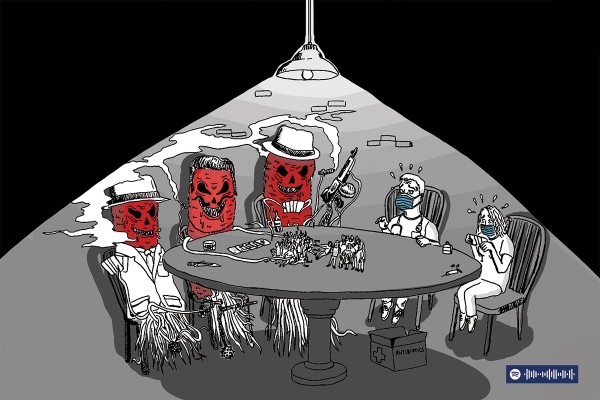
But it’s not just resistant strains that are causing concern. Every time we use antibiotics, we make the general population of harmful bacteria just a little bit stronger. So, next time we take antibiotics, that first line of defence has to be just a little bit stronger as well. We’re caught in a microscopic arms race, with each side bringing bigger and bigger guns to the table, and your helpful bacteria can get caught in the crossfire. Take your gut, for example. Bacteria live there that produce neurotransmitters, the stuff that regulates brain function. When you take an antibiotic – any antibiotic – you’re essentially swallowing gut napalm. And the stronger and stronger that we have to make that first line of defence, the more and more of your helpful bacteria get burned away.
Critic also spoke to George, who studies a particularly gnarly strain here at Otago. She told us that the World Health Organisation is most concerned about what they call the “ESKAPE” pathogens, six pathogens that each correspond to a letter in the acronym ESKAPE (Staph stands for ‘S’, for example). George said that the Uni gets samples of bacteria from people at the hospital and all over New Zealand, and that “some of the samples we get out of patients are reeeally nasty”. She said that when a new antibiotic is tried on a sample, an “R” is put in the spreadsheet if it’s found to be resistant. “And looking at some of those results, it’s just R, R, R, all the way down the sheet”.
George said that of all the global crises, bacterial resistance was pretty close to the top of their concerns. “You should 100% be worried about this. And climate change. And all of the plastic in the ocean. There’s a lot of things to worry about and this is just one of them”. George said that, like the burgeoning climate crisis, “We’re approaching the post-antibiotic era pretty rapidly at this point. That era meaning that if you get an infection in your foot, you'd probably need to get your foot amputated instead of just taking some amoxicillin. We’re fucked six ways from Sundays, this is one of the ways we’re fucked.”
From the very beginning, scientists have been warning people about the dangers of antibiotic resistance. Any time you prescribe antibiotics, you are at least somewhat increasing the likelihood of helping to create a newly-resistant strain. But how are we meant to judge the current and dire need of someone who needs antibiotics against the future wellbeing of our communal immune systems?
“I would say the last two years have shown us that as a global community we suck at dealing with infectious disease threats”, said Brian. “New Zealand really needs to break away from the rest of the world and get a hold of this. And that starts here. Dunedin has lots of medical professionals doing exactly that. We need to support them, and we need to be good antibiotic stewards.” And you need to make sure to finish your prescribed course of antibiotics.