Contraception: The Intra Uterine Device
One of the best types of contraception that hardly anyone seems to be using
Critic also spoke to Dr. Jennifer Ogilvy, GP at Dunedin’s Student Health Clinic. She believes it is important that women are made aware of all options available because “few 18–25-year-olds at university will be planning to start a family and an unplanned pregnancy can be devastating for young women and their partners. Any woman in a heterosexual relationship is potentially at risk of pregnancy, even if they are not having full penetrative sex.”
In 2013, there were 14,073 abortions performed in New Zealand, with the highest abortion rate occurring in women aged 20 – 24 years. Although this is the lowest rate in New Zealand since 1995, it is still a significant number. With the right contraception methods used, this rate could certainly be decreased further.
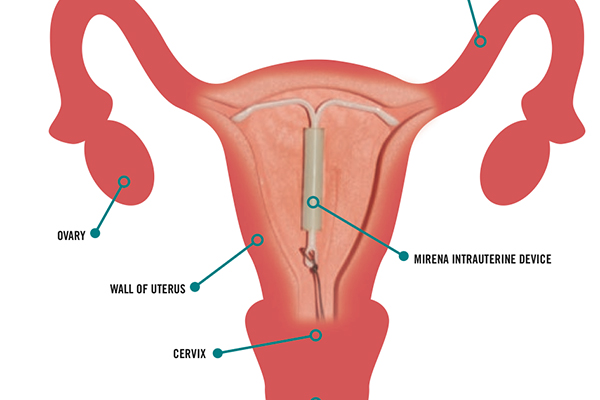
The IUD is a small device, available in two forms, which is placed inside the woman’s womb. At the end of the device are small nylon threads, which are required for removal. These threads come out of the cervix and curl up inside the vagina. Unless you are checking for threads, it is very unlikely that you can tell it is there. It is also very rare that during intercourse, a partner will be able to feel it. Tampons can still be used with the IUD.
The Mirena IUD contains progestogen, a hormone that is slowly released over time, which stops the sperm from travelling towards the egg. There is also a copper IUD available, which has the same effect as the progestogen. In the rare case where the egg does become fertilised, both types of IUDs then stop the egg implanting into the womb. This is so effective that the copper IUD can also be used as a form of emergency contraception after unprotected intercourse has occurred.
The IUD comes under the umbrella of the LARC (long acting reversible contraception) group, along with implants such as the Jadelle. Perhaps the greatest advantage is that “it is a fit and forget contraceptive,” says Dr. Roke. After insertion, the copper IUD begins working straight away, but the Mirena takes seven days to become effective. Both forms provide the woman with 99 per cent protection for the next five years. No further check-ups or maintenance is required. The failure rate for an IUD is less than one per cent per year.
In terms of the insertion process, the IUD is fitted by a doctor or nurse and usually takes around five to ten minutes. Dr. Roke said that there is a little bit of discomfort when inserted, she described it as “a little like nasty period pains, but some people may find it a bit more painful.” In regards to how long the pain lasts, Dr. Roke said “the acute pain is just while it’s being put in, then it tends to get a bit niggly and crampy like a period pain for a day or two.” Spotting is also likely to occur.
Family Planning Clinics are the most cost-effective option for young New Zealanders wanting to have an IUD put in, or to even enquire about other forms of contraception. If you are a New Zealand resident under the age of 22, a consultation with a doctor or nurse is free. For a New Zealand resident over the age of 22, a consultation with a Community Services Card is five dollars; without a card, it is $27. The copper IUD is completely subsidised, however the Mirena will cost $333. Contraceptive implants such as the Jadelle cost $17 for insertion. Other contraceptives are free, however a five-dollar prescription fee at a pharmacy may apply. Further information can be found at Family Planning, 95 Hanover Street Dunedin.
With over 5,000 IUDs being put in through Family Planning during the 2013 calendar year, it is steadily becoming one of the more popular forms of contraception. Dr. Roke pinpoints this increase to two factors: “We’ve been talking about them more, but also partly because research has shown that the myths surrounding the IUD have been proved to be wrong.” It is commonly thought that people who have not had children yet should not use the IUD because it could cause infertility. Another myth is that they regularly cause infection. However, “it’s much clearer now that those ideas are not correct.” There is also no evidence that the IUD causes acne, headaches, breast tenderness, nausea, mood changes, a loss of libido or weight gain.
Dr. Roke assured Critic that the IUD’s effect reverses as soon as it is taken out, so there are no long-term fertility problems. She did note, however, “If you catch a sexually transmitted infection you’re more likely to have problems with fertility.” On this note, she insisted the IUD “doesn’t protect you against sexually transmitted diseases or infections, so you need to use condoms if you are at risk.”
As with any form of contraception, there are negative consequences to the IUD. There is a one per cent risk of infection when it is first put in. The two different types of IUD can also have different impacts on a woman’s menstrual cycle. Dr. Roke says the copper IUD tends to make periods a bit heavier, longer, and more painful. Spotting, light bleeding, heavier or prolonged bleeding is common for the first three to six months after insertion. The Mirena tends to reduce your periods, or even stop them completely. For the first three to six months, there may be light bleeding or spotting but after this period, it is common to have no bleeding at all.
Although IUDs are effective at stopping pregnancies in the womb, they do not necessarily stop the ones that could have been settling into the tube pre-insertion, which Dr. Roke says “can be quite dangerous.” There is also a slight chance the IUDs can perforate the uterus or go out of the uterus and enter the stomach. In these cases surgery may be required. However, the chance of this is approximately one in every 1,000. There is also a five per cent chance that the IUD can completely come out, although “this is not dangerous, it just means you lose your contraception.” Copper IUDs can also cause an allergic reaction, but this is extremely rare. Dr Roke also advises that if women have symptoms of any infection, they should have treatment before an IUD is inserted.
Dr. Roke said “[Family Planning] very much encourages IUDs as a contraception method. They work out [to be] much more effective as you don’t have to remember a pill or get out a condom, you also don’t have to remember to go back for an injection.” She also believes any form of preventative contraception is a safer option of birth control than continuous use of the Emergency Contraceptive Pill (ECP). It has been found that for women weighing 70 kilos or over, the ECP is much less likely to be effective. She says that women over 70kgs generally have to have a copper IUD put in to prevent that egg settling into the womb. “If you have a failure rate of a couple of per cent each cycle and each time you take the emergency pill, then over a year that equals to be quite a lot,” said Dr. Roke. Most women have thirteen menstrual cycles per year, so “that equals about 26 per cent chance of getting pregnant that year.” She says “[The ECP] is not a very good contraception method on-going, but it is wonderful on the odd occasion.”
In regards to the student population, Dr. Roke says that it is extremely important for students to practice safe sex. “There are two parts to it: pregnancy and the threat of STIs.” She said that “each contraceptive suits a particular group” and recommends that people look through a list of the different forms of contraception and decide what would work best for their sexual relationships.
In regards to contraception methods, Dr. Ogilvy at Student Health says condoms are effective for prevention of STIs, but not particularly effective as contraception. “The combined oral contraceptive pill, the injection, the implant and the IUD all offer very effective contraception but afford no protection against STIs. Generally we would advocate an effective method of contraception such as pills, injection, implant or IUD combined with using condoms.” Dr Ogilvy also recommends that both partners should have regular STI checks, then “if they are both clear and are only having sex with each other, then and only then, is it reasonable to think about not using condoms.”
Dr. Ogilvy said “any of the doctors and nurses at Student Health are happy to suggest suitable methods of contraception for each individual. We try very hard to educate students around safe sex practices and help with informed decisions regarding contraception, use of condoms, regular cervical smears and STI checks.”
“Queer or straight Student Health staff are here to help with information and advice around all aspects of sexual relationships – safe sex, potential abuse, contraception, STIs, etc. All consultations are confidential and non-judgmental,” says Dr. Ogilvy.