BODY COUNT: What happens to the bodies donated to the Otago medical school?
Susan Smirk investigates how they come to be donated and what happens to them, as well as introducing a confronting new Otago documentary on the death-cycle of the human cadaver.
Why dissection?
The staff, students, and even those who bequest their body to medical science all acknowledge that human dissection is a crucial learning experience. Medical School Dean Professor Helen Nicholson notes that even the best computers or models are no comparison to the real thing. Yet Otago is one of the last medical schools in the world to allow human dissection. This is often because of health and safety issues, or cultural and religious beliefs. However, it is also very much related to the cost and space needed for working with cadavers.
The University of Otago received its first body for study in 1943. Today Otago accepts 100 registrations and 40 bodies annually. Auckland School of Medicine accepts over 30 bodies a year from willing donors. Back in the dark old days of seventeenth- and eighteenth-century Europe, methods of procuring bodies for study were not quite so savoury. In fact, the medical profession pioneered a proud tradition of body-snatching and grave robbery. The only exception was during the reign of Henry VIII, who decreed it legal for surgeons to use the bodies of up to four criminals a year.
Otago has no problem obtaining the number of bodies they require each year, which Nicholson puts down to the generosity of New Zealanders. She is quick
to note that her film on donating to science is in no way intended to recruit new donors. Nevertheless, she admits that it has caused an increase in bequests.
From life, to death, to dissection
To donate your body to science, you must have all the paperwork filled out before death. The Human Tissue Act 2008 governs the bequest of bodies for anatomical study. Under this Act, if any close family members object to the donation after your death, the Department cannot accept it.
You can't donate if you have:
• an infectious disease
• have had complicated or extensive surgery within a month of death
• displayed a rapid onset of dementia
• body weight greater than 90kg
• undergone a post-mortem
• lived in the UK, France or Ireland for over 6 months, between 1980 and 1996.
Once declared dead, bodies destined for the Medical School must be specially embalmed within 24 hours. Since the only places with facilities to do this are Dunedin, Christchurch, and Nelson, only those living in these regions can be donors, and if the person dies outside the accepted “catchment” area, the body is unlikely to be accepted. Once embalmed, the body is placed in a specially constructed container which is apparently 'more suitable' than a usual casket. The department pays for embalming, but the budget doesn't stretch to cover a formal hearse for transportation. They also pay for eventual cremation. The body is disposed normally no longer than 18 months after death, and the ashes are scattered at Anderson's Bay Cemetery, unless the relatives request to have them returned. Meanwhile, the bodies are studied by medical, dental, physiotherapy, physical education, and science students, as well as by some academic staff doing research.
Given the time imperative, holding a funeral with the body present is not a possibility for friends and family. Funeral directors have often noted how difficult it is for the family to grieve without a body. However, the Otago Medical School holds a Thanksgiving service each year for the families of donors. According to relatives, this does help to provide a much needed sense of closure. It also lets the medical students and staff personally meet and thank the families. It is this service which provided the foundation for a film on medical dissection to be made.
The film: behind the scenes
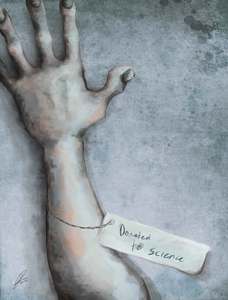
Title: Donated to Science
Tagline: Humanity is more than skin deep
“It's not every day that you make a film about human dissection,” says co-producer Professor Helen Nicholson to the motley audience of a public screening last Saturday. Indeed, this is the first film of its kind, and undoubtedly a risky project. Nicholson says her main motivation for wanting to see the film made was simply to educate the public, families, potential donors, and even funeral directors about exactly what happens to the bodies the Medical School receives, and to “debunk some of the horrible myths.”
Professor Nicholson co-produced the film with Dr. Paul Trotman, who also directed it. Trotman went through medical school himself once upon a time; he describes himself as “the world's worst anatomy student.” After graduating he headed to Britain to pursue an interest in entertainment. After several near-brushes with success writing sitcom pilots for the BBC, he returned to New Zealand frustrated. Eventually, through what Trotman tells Critic was “a whole lot of very lucky circumstances,” he fell into employment with Natural History New Zealand (NHNZ) and got a crash course in documentary film-making, with a focus on science and medicine. The idea for this film, Trotman says, “came out as a whole idea, except it had the addition of 'but there’s no way anyone will ever let me do it.'” He was working on a film about organ donation when he realised that a similar story could be crafted by following the journey of the body bequeathed to medical science. After his initial certainty that the idea would be rejected by the powers-that-be in the Medical School, Trotman says that Helen Nicholson's response made his jaw drop. “I made an appointment to go see Helen, who I'd never met before,” Trotman says. “I walked in and said 'this is what I'd like to do' and Helen just said 'yes.'” He says Helen then made good of her promise to deal with the ethics committee – a difficult, nine-month process.
The Medical School was mostly supportive, and filming took place over the next two years. The long time frame and manifold funding issues meant that Trotman was often wielding the camera himself. But when the film was finally complete, selling it proved “incredibly difficult,” says Trotman. TVNZ said yes, then changed their minds. TV3 then said yes, then no, then finally agreed. The TV3 showing was extremely successful, making the film the highest rated documentary to screen that year, and the highest rated programme screening that night (ironically even outranking House). 720 000 people tuned in to watch it. Despite the documentary’s commercial success, though, they have had little luck selling it elsewhere in the world, or getting it accepted at film festivals.
Nevertheless, the reaction to the film in Dunedin has been very positive. “It's just so good being in the audience when people are watching it, because they laugh at the places where they are supposed to laugh, they go really quiet at the places where they are supposed to go really quiet. You can't make a film which is just the same note all the way through, you have to have some serious stuff, some sad stuff, some funny stuff, and some stuff where you think, 'Ohh, I'm not quite sure about that.' It gives it balance. It's pretty hard to make dissection funny, but because of things that people said, we pulled it off.”
Trotman is planning a sequel, which follows the same students (now in their fifth year) through their experiences training on the wards. It will show, he says, “a lot of things people don't usually see.” Trotman is also currently editing a film on pig-cell transplants in Auckland, and is interested in making a film on animal research. Meanwhile Donated to Science has featured in the Dunedin International Science Festival, where audiences were apparently eager to embark on the morbid and emotional journey through the bequestees life, death and dissection.
The film:
“Sensitive and respectful,” once audience member calls it. But it was also raw, emotional, explicit, and very compelling. Firstly, we meet the donors – in rambling interviews these charismatic, loveable individuals are asked about their lives, their decision to donate, and even which body parts they think are the best (“Well it'd have to be my heart” says one “because my brain is buggered!”) Next, we meet the medical students, on their first day in the dissection room. Prof Nicholson said that the film really shows “how amazing our students are.” It also shows just how challenging this part of the course really can be. The range and depth of emotions the students show on screen is stirring: the horror at their first glance at a corpse; reluctance to make the first incision into cold human flesh; wonder at the complexity of the human body, and eventually determination to make the most of the generosity of the donors. “Nothing quite prepares you for cutting through someone else's skin,” says one student. But even the most seasoned staff do not become entirely desensitised to the reality of their work. One explains, “every year there is one or two cadavers that affect you.” Another notes that the work became harder when they experienced a death in the family themselves. But all saw human dissection as a vital, valuable learning experience that stays with students both emotionally and intellectually as they graduate and begin careers as doctors. “Every single heart will be the heart of the first body you dissected,” said one staff member.
For the students, and for the audience, it is an experience that explores and tests their deeply engrained notions of personhood, the sanctity of the human body, and our own mortality. To explore death with a human body in such intimate, personal, and often violent ways crosses many social taboos, no matter how logical and secular our society may claim to be. One student says, “it felt like stepping over every boundary there possibly was.” Even watching the film was often highly uncomfortable. Seeing the flesh peeled slowly back from the face; watching students take a hammer and chisel to bone; even simply the sight of the emaciated body of a cancer patient is unsettling.
Director Paul Trotman explains to Critic, after the screening, how the poignant ending of the film came about. It wasn't part of the original plan, he said. One of the lecturers commented to him that he was in a unique position, having met the donors before their death, and then also seeing their bodies studied afterwards. Trotman narrates, “I suddenly realised that we could reverse that! We waited until the students had finished, and asked them if they wanted to see the interviews with the bodies they had dissected. Every single one of them said yes [...]We literally took them from seeing it, sat them down, and interviewed them. We had a very, very powerful reaction.”
Many of the toughest students cry as the camera rolls. After two years spent dissecting a body, and wondering about the donor’s life, “we got quite attached to our guy,” says one student with quiet sincerity. Another struggles to speak through tear: “I am mourning for the loss of a death I didn't know, a life I missed out on ... and a body I destroyed. And the worst thing is that's what he wanted. He just wanted us to learn.”
(sidebox) Get the film:
• University Bookshop
• Marbecks.
• prnfilms.co.nz
(Potential side-box) Who would do that?: a profile of donors
This year, a survey of those who bequeathed their bodies to Otago University was conducted. The study was a repeat of a similar 1992 study, and only the fourth of its kind in the word. Researchers Kathryn McClea and Mark Stringer of the Anatomy and Structual Biology department sent questionnaires out to randomly selected bequestees, to compare today’s donors to those of 1992.
They discovered:
• Most people bequeathing their bodies were over 50 years old – the oldest was in her 90s, the youngest was a male in his 20s.
• Few bequestees were in healthcare jobs, and none were medical doctors.
• Slightly more men than women donated.
• Reasons for donation have changed slightly since the 1992 survey, showing that most are now better informed about how their body would be used.
• 90 percent of respondents said their purpose in bequeathing their body was to aid medical science. The next most common reason was gratitude to the medical profession for past or current services. 18 percent also reported that they were donating partly due to a dislike in funerals, and six percent cited the cost of funerals as a reason.
• Nearly 40 percent of bequestees came from families where others had also donated their body.
Potential side box, or insert somewhere else you want
A Maori ceremony, or whakawatea, is carried out at the beginning of each year in the dissecting room that holds the covered bodies that will be studied. It is described as a “clearing of the way” and is supposed to help Maori students who will attend classes there come to terms with the death, and is not intended to have significance for the individual bodies.