THE GRAVE HISTORY OF MEDICAL CADAVERS
For over two thousand years, cadavers have been involved in science’s greatest accomplishments, especially in the field of medicine.Herophilus, the “Father of Anatomy,” lived in Egypt in 300BC and was the first recorded physician to have dissected human bodies. The use of cadavers led to rapid improvement in the anatomical and physiological knowledge of the human body, and altered the course of medical pursuits throughout the world.
Up until the eighteenth and nineteen-centuries, criminals were the main source of cadavers in medical schools in England and Scotland. People rarely donated their bodies for research because – seemingly paradoxically – it was widely believed that despite such generosity, the souls of dissected bodies could not go to heaven.
When the number of executed criminals decreased, it became commonplace to remove corpses from graves in order to satisfy the demand of medical schools. It’s wrong to label “body snatchers” as “grave robbers,” however, because taking a body from its grave was not considered stealing (as long as the snatcher didn’t take clothing, jewelry or other material possessions).
In fact, some anatomy professors encouraged this practice of “grave digging,” and allowed their students to pay for tuition in corpses. During this time, self-dubbed “Resurrectionists” made it their profession to exhume corpses and then sell them to medical schools for dissection.
This trade was short-lived, however, due to the Anatomical Act of 1832, which stipulated that only licensed “teachers” were allowed legal access to corpses for anatomical examination and dissection, provided that “no relative [of the corpse] objected.” This meant that medical schools were granted legal access to unclaimed bodies – often corpses of those who had died in prison or workhouses.
Disposing of dissected bodies was a problematic issue for many anatomists. It’s rumored that remains were secretly buried beneath medical schools, consumed by purpose-kept vultures, or even given to zookeepers, as feed for carnivorous animals.
By the end of the nineteenth century, processes of embalming and preserving dead bodies became more advanced. This led to a reduction in medical cadaver turnover, as students and researchers were no longer in a race against decomposition.

BODY BEQUESTS AT THE UNIVERSITY OF OTAGO
So, where does the University of Otago fit into the plot of all this?The Otago Medical School has used bodies for dissection purposes since 1875. Initially, the cadavers were sourced from The Benevolent Institution (poor house), and later from various mental hospitals around the region. The first official bequest to the Otago Medical School was recorded in 1943, and – although unclaimed bodies from mental hospitals continued to be used until the late 1950s – altruistic donation has since become the sole source of medical cadavers. All aspects of the bequest programme are now monitored by an Inspector of Anatomy (a senior member of the New Zealand Police) and governed by the Human Tissues Act 2008.
Donated bodies are predominantly used by students of medicine, dentistry, physiotherapy, physical education and science, as well by as researchers undertaking projects on cadavers. The Department of Anatomy receives more than 100 registrations each year, and more than 40 cadavers, which just about meets the University’s requirements.
Unlike family debts and illegitimate children, intentions of body donation can’t be introduced at one’s deathbed. According to the Human Tissues Act, even if the donor’s intentions were clear, a family member’s objection can prevent the Department from accepting the body. The registration process for bequests is therefore both lengthy and thorough, to ensure that donors and their families are fully informed about the situation, and actually willing to go through with it. Most donors are aged in their 60s or 70s when they first contact the Department, and apparently there are roughly equal numbers of male and female donors.
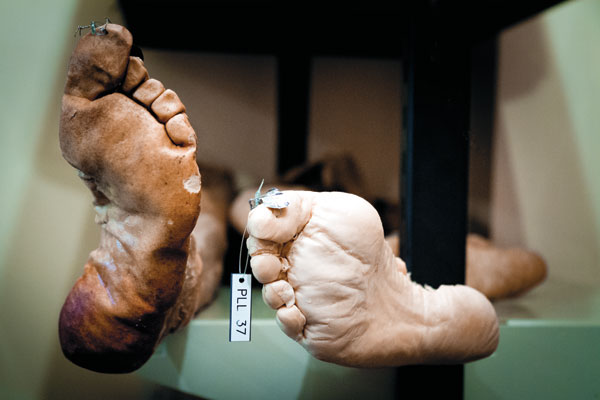
Once a donor’s death has been confirmed and their body accepted, the cadaver is removed for embalming, and then transported to Dunedin. To allow for adequate fixation to take place, the Department has elected not to begin dissections until a period of six months has passed from the time of embalming – leaving plenty more than the traditional three days for one’s soul to move on.
Although all donations are appreciated, not all can be accepted, due to restrictions surrounding the University’s bequest procedures. Donors are informed of these restrictions at the time of making their bequest, and families are informed of the importance of a “back-up” plan, lest the donation can’t proceed.
The Department isn’t able to accept a body if, for example, the donor has contracted certain contagious diseases, or if they’ve developed dementia within six months of death, or if they’ve undergone major surgery within a month of death. Bequests aren’t accepted from outside the Dunedin, Christchurch, Nelson or Invercargill areas (due to embalming specifications), and the donor can’t also give their organs for transplantation. Despite donor shortages at many medical schools elsewhere in the world, the generosity of Kiwis is such that our Department has on occasion in the past been forced to decline body bequests.
At the end of each year, all remains not to be retained are placed in coffins, cremated, and the ashes are scattered on a commemorative rose garden at the Anderson Bay Cemetery in Dunedin. There is a similar garden at the Nurses’ Chapel at Christchurch Hospital, also dedicated to the memory of the donors.

MEDICAL CADAVERS: THE STUDENTS’ PERSPECTIVE
One of the main motivations for potential body donors is the knowledge that what they’re offering students is an irreplaceable learning tool.Dr Paul Trotman, director of the recent Otago-based documentary Donated to Science, acknowledges the unparalleled benefits of the cadaver experience:
“The real thing that comes across is that students learn far more than just anatomy from doing dissection. This is their first patient. They learn compassion, they learn about dealing with death, they learn about themselves, they do a lot of growing up, and it changes them. It’s their first step to becoming a doctor.”
Campbell (not his real name), a third-year medical student, shared his cadaver experience with the Critic:
“As a learning tool… The cadavers are definitely irreplaceable. We’re always looking at textbooks, but to use real bodies is much more helpful. With the hands-on experience, you actually get to appreciate how complex the human body is.”
In order to prepare them for working with their cadaver, medical students are given lectures on the ethical treatment of human materials, and are encouraged to watch Trotman’s documentary, so that they can view the reactions of other students. Campbell says that, “…we also had this ceremony where we walked around all the cadavers, just to say thanks to them.”
The University encourages students to reflect regularly on their feelings and emotions when dealing with cadavers. Each year among the dissection classes, there tends to be a few fainters, a handful of criers, and many who choose to stand back and observe rather than participate. As Campbell says, “We take turns at dissecting. Those that don’t want to dissect, if they can’t bring themselves to do it, then they don’t have to. At the beginning [of second-year] about a quarter of the class just watched. But as the weeks went on, more and more students started participating in dissections.”
When it comes to slicing through human skin, it seems that each student develops their own methods for mentally protecting themselves. Campbell admits, “…I thought it was a bit weird, and a bit strange, at first. [The cadavers] don’t look like us, because they’ve been preserved, and because most of them are much older, so I was sort of able to distance myself from the experience. Although, their hands… I don’t know what it is about hands, but that kind of got me at the start. They looked so normal.”
Fortunately, students don’t need to worry about recognizing any faces on the dissection tables: “They do background checks to make sure that students won’t know any of the bodies, because that would be disturbing.”
Interestingly, Cambell thinks that using cadavers in learning encourages the students to consider donating their own bodies to science: “From the majority of people that I’ve talked to, they all enjoyed the experience of doing [the dissections], and really appreciate the value of it as a teaching tool. I think many of us lean towards wanting to donate our own bodies, to help out future students, because it’s such a good experience.”
Cambell says that his teachers, “…always reinforce the importance of respecting the bodies, and of being grateful for their donation.”
Every year the Department holds a thanksgiving service, for family and friends whose loved ones donated their body. In absence of a funeral, it offers closure for those who knew the donors during their lifetime and – in the cases of students – those who appreciated them after their death.
MEDICAL CADAVERS: ETHICAL ISSUES
While many medical schools overseas are replacing cadavers with textbooks and computer resources, the University of Otago is renowned for valuing human material in the teaching of, and researching into , human anatomy.Such precious resources as human materials require weighty ethical consideration, yet it appears that this hasn’t been appreciated until relatively recently. Professor Gareth Jones, previous Head of Department of Anatomy and current director of the Bioethics Centre at the University of Otago, strongly values an ethical perspective when dealing with cadavers: “For so many anatomists, wherever you go, they simply said that what we’re doing is legal, and we’re conforming to that. Which was true, but they weren’t asking the question, ‘why?’ This seemed to me to be a very basic ethical question.”
The most resounding of such ethical concerns, according to Professor Jones, was the appropriateness of using “unclaimed” bodies as medical cadavers. As he says, “Those [unclaimed] bodies tended to be from the poor, the disadvantaged, the outcast, and generally the most vulnerable people of society. Altruistically bequeathed bodies seemed to me to be far superior, ethically.”

Although the University of Otago now relies solely on bequeathed bodies, Professor Jones aims to get the anatomical profession worldwide to think seriously about the repercussions of using unclaimed bodies. “[Use of unclaimed bodies] opens the door to very dubious, ethically slippery circumstances.
So why is it important to place all of this emphasis on respecting the bodies of the dead? It seems that we have an innate sensitivity towards dead bodies, even those of people who we didn’t know. Professor Jones says that, “…we relate a dead body to the life of the person who inhabited it. It represents a link between the living and the dead, in terms of memories, and also what the body itself stands for, especially for the family of the deceased.”
Indeed, the interests of the body’s family are granted high regard in matters concerning body bequests – as I’ve already mentioned, they have the power to veto the whole donation process. Is it really fair to give the wishes of the living such weight over the wishes of the dead? Professor Jones thinks that, “…ethically, this is an area that’s full of tension. And it’s exactly the same when it comes to donation of organs… If the family says ‘no’, then they override [the intention of the donor]. The families’ wishes and feelings are placed above those of the donor, and that’s a highly debatable issue.”
Professor Jones insists though, that it’s important to realise that the gift of a body is not just a gift from the deceased, but also a gift from the deceased’s loved ones. Once again, this brings us back to the central motivation of altruism – an attitude which Professor Jones stresses is important throughout all aspects of medicine: “The issues that we encounter here are very similar to the issues that we encounter in clinical medicine. And that the basic ethical value of altruism really was, and should be, the main driving force.”
Donors have various reasons for wanting to gift their body, but often it’s a desire to “give back” to a profession, which has, in some way, aided their lives. Others claim that they simply don’t like the idea of being “left to rot” in the ground. Whatever the donor’s reason, students, teachers, and the public, are truly indebted to them for their magnanimous final act.